Yummy!
Archives: Generic Topics
Ways to ease breathlessness
Pick and choose the strategies below you think will work for you. Try to practice these when the person you support is feeling ok. Remember many of these strategies can be used anywhere – whether you are home or out and about.
Handheld fan / cool moving air
A handheld fan looks very simple but it’s a very good way to get cool air on the person’s face when they are breathless. Cool air on the face is a way to calm down and relax and can reduce breathlessness. A handheld fan with three, soft paddles is recommended, although any type of fan can be helpful.
Get them to hold the fan in close to their face and mouth, and slowly move the fan from side to side, making sure the flow of air covers the nose, mouth and cheeks. They can also use this fan while using nasal oxygen. While they use the fan, encourage them into a comfortable position that eases breathlessness. See below for more ideas on positions to ease breathlessness.
You can also watch a video on how to use a handheld fan to reduce breathlessness over on the Breathlessness Intervention Service (BIS) website.
You can also try cooling their face with cool flannels or a water mist spray.
Positions to ease breathlessness
There are many different positions you can encourage the person you support to try that may help relieve breathlessness. There are resting positions, positions after activity and positions using walking aids.
There is no one position that works for everyone, so experiment and find out which suits them best. Ask them to try sitting or standing, leaning onto something like a rail or chair or leaning back onto a wall.
Leaning forward is often helpful for people with breathlessness. There are lots of ways you can use this position when doing everyday tasks. For example, using a trolley often helps people walk for longer without becoming breathless when out shopping. Walking frames can help in the same way too. There are kinds of exercise equipment like bikes, that also encourage leaning forward and can help exercising with breathlessness.
Some examples of positions you can encourage them to use that relieve breathlessness:
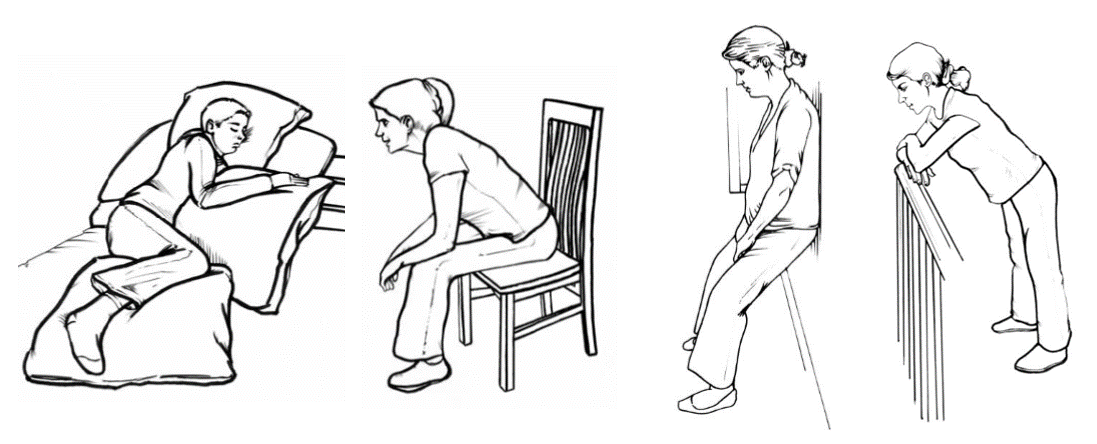 (Images sourced from the Breathlessness Intervention Service (BIS) website)
(Images sourced from the Breathlessness Intervention Service (BIS) website)
See some more ideas of positions that can help ease breathlessness over on the Breathlessness Intervention Service (BIS) website.
Rectangle breathing
Rectangle breathing is a technique you can use with the person when they may be feeling panicked or breathless. It can help to look at something with a rectangle shape while doing this breathing such as a picture or mirror frame, computer screen, a door or even a book.
Start by trying to breathe from your stomach, and as you do, follow the sides of the rectangle with your eyes. Try to slow the speed of your eyes to follow the edge of the shape of the rectangle and to slow your breathing, breathing out along the long edge, and breathing in along the short edge.
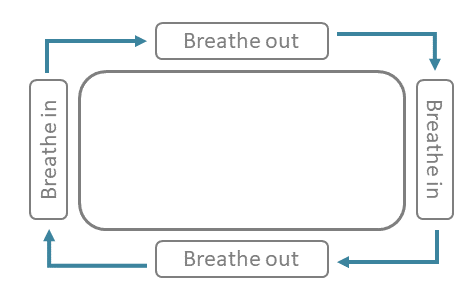
The feelings of panic and breathlessness may not fully go away after using this technique only once, so encourage them to use it several times until the panic has goes away – go round and round the edge of the rectangle. Encourage them to practice.
Medication
Make sure they uses their reliever inhaler if they have one. If this makes their mouth dry, sipping cool water can help.
Your healthcare professional can also recommend the best ways to use inhaled medications that may help.
Acupressure
Acupressure involves putting pressure on specific points of their body which can be helpful when they are feeling anxious and stressed.
Using the palm of your hand, firmly stroke down either one of their arms all the way to the end of the thumb. Also try rubbing the top-middle of their back.
Watch a short demonstration on how to use acupressure to relieve stress and breathlessness in the video below
Relaxation
It’s important for you and the person you support to relax and manage stress every day, not just during times of breathlessness and panic. This can make sure that your baseline, day to day levels of stress are lower and may mean that having a panic or breathless episode is less likely.
It can help to do things like listening to ‘body scans’ and ‘guided visualization’ relaxation exercises together.
Try the ‘Letting go’ relaxation script from the Breathlessness Intervention Service (BIS).
The Breathlessness Intervention Service (BIS) and Macmillan Cancer Support also have other relaxation exercises that can be helpful for anyone with breathlessness. There are many other relaxation exercises you can find by searching on the internet, especially YouTube.
Click here for a printable version of this page (PDF, 478KB)
Would you like to look at another support topic?
Page last reviewed: 08/05/2020
Stress and breathlessness – an unhelpful cycle
Stress is a common feeling we all have from time to time. It is impossible to take away stress completely, but there are lots of ways to manage stress levels when they start to get out of hand.
Often we become stressed when we think about things that may happen in the future. This worry can then cause changes in our bodies like tense or tight muscles, an upset stomach, dizziness and shallow, faster breathing.
It is common for people with health problems and their carers to feel more stressed than other people. This is because they are faced with extra challenges, day-to-day.
Stress can be particularly unhelpful for breathlessness because together they can create a vicious cycle, feeding one another.
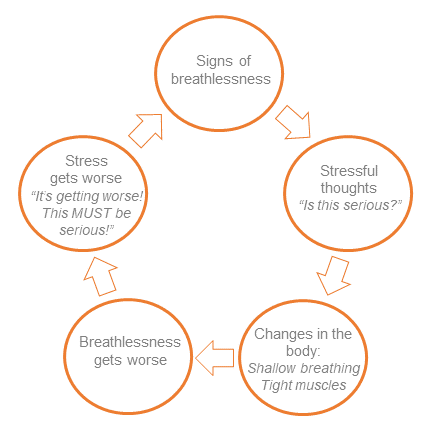
Chris notices he is feeling breathless.
He worries that he might not be able to catch the next breath and starts to feel stressed and anxious.
As part of the stress, Chris’ muscles start to tighten and his breathing gets faster. These bodily changes caused by stress make it harder to breathe and lead him to feel even more breathless.
As the breathlessness gets worse, he becomes more and more worried about not being able to breathe. Chris is stuck in a stress-breathlessness cycle.
What you can do to help the patient
Remember that if the patient is stuck in this stress-breathlessness cycle, there are lots of things you can do to help them break out of it.
Would you like to look at another support topic?
Page last reviewed: 08/05/2020
Our support topics
Listed on the left are the main topics carers told us they want to know more about.
Within each you can see, hear and read advice from experts, carers and patients.
To access this advice, click on the relevant button on the left.
Make more of an intro page. Perhaps have images of the buttons on the left under the text above.
Pacing
Pacing is about:
- trying not to rush things or do too much at once – these can tire you both out, making you both feel worse in the long run
- creating a balance between being active and resting
This sounds simple, but there are a couple of ‘traps’ that carers and patients can fall into which can lead to problems later on:
Trap 1: Boom and bust
Boom and bust is a common cycle that people with health problems can find themselves in. The diagram below explains why this cycle can be a problem:
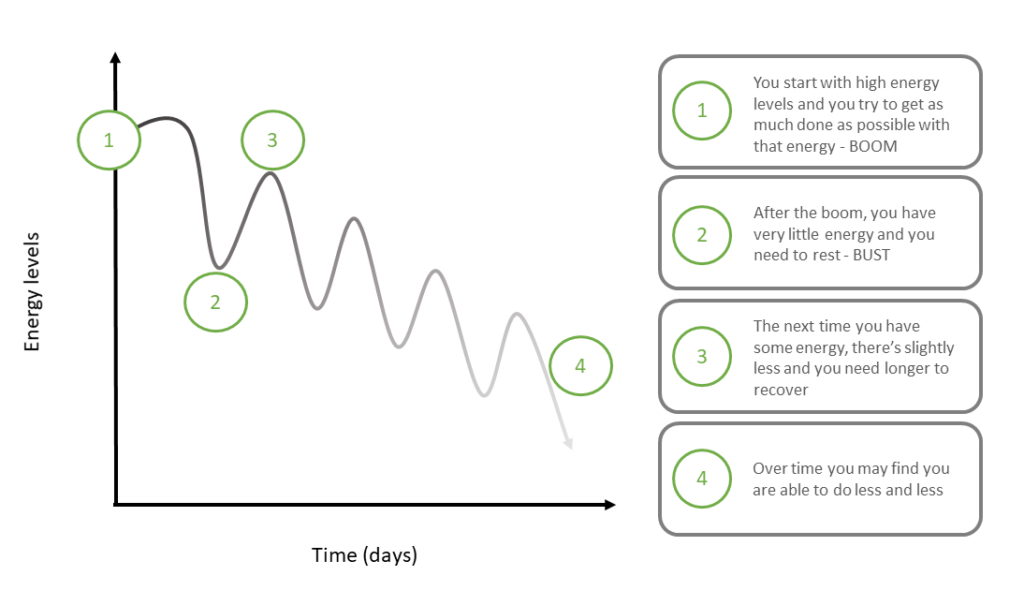
Trap 2: Resting too much
Energy levels can be unpredictable for people with breathlessness.
It can seem hard to tell which activities will make them tired and which won’t.
For patients it can be tempting not to do anything much at all and just rest. Sometimes carers also take over and do everything for the patient.
Too much rest without activity is actually unhelpful, as it can mean losing fitness and muscle which cause people to feel even more tired.
What you can do to help the patient
- To avoid a boom and bust, where you might do a lot on one day and then rest for several days following, try to keep the amount of activity you and the patient do stable. Think about doing as much on a lower energy day as you do on a higher energy day.
- Try to break down big or long jobs into smaller or shorter tasks with regular breaks in between.
- While it can feel frustrating, and may take longer to do things this way, the patient should have more energy afterwards and avoid the ‘bust’ part of the cycle.
- It’s also important to encourage the patient to do things for themselves. Not enough activity can lead to longer term problems as their muscles weaken and they may lose fitness.
For more ideas of ways to keep active with the patient see Keeping active.
In the video below, carers and patients discuss how they use pacing to manage their activities with breathlessness
Would you like to look at another support topic?
Page last reviewed: 08/05/2020
Permission
Supporting people with breathlessness to live a fulfilling life, and to do everything you need to get done, can be challenging.
Carers and patients can put a lot of pressure on themselves to do things in the same way as other people or to do things in the way they did before the patient had breathlessness. Because of this, it is common for carers and patients living with breathlessness to feel frustrated at times.
In reality, everyone’s experience of breathlessness is different and everyone is able to do different amounts.
What you can do to help the patient
- Giving yourself and the patient permission to do things in a new way – your own unique way – can help take off some of this pressure
- Giving yourself permission to do things differently can also help you do the other 5 Ps
- It’s also important to give yourself permission to look after your own health
- Focus on what you and the patient are able to do, rather than on what you can no longer do
- Try to be patient with one another and talk to each other if you are feeling upset. More often than not, if you are finding something difficult, the patient will be struggling with it too.
Would you like to look at another support topic?
Page last reviewed: 08/05/2020
Problem solving
Problems will arise and plans are likely to need to change when you are living with breathlessness – even with the best prioritising and planning.
Being able to problem-solve together to overcome these problems will help get you both back on track.
There are lots of activities you can do together, and some might even help the patient’s breathlessness.
Steps for problem-solving together – Ask yourselves ‘what is the problem?’ Does it help to break it down into smaller pieces? – Ask yourselves ‘what might help solve this problem?’ Can someone else help or give advice? Try to think of solutions with the patient that meet both of your needs. – Decide which solution is best. It can help to think of the pros and cons of each. Listen to the patient’s concerns. The solution: contact the doctor to see if a phone consultation or home visit can be arranged.Have you tried...?
Sarah needs to see the doctor for a new prescription but she can’t travel as she is too breathless
Rebook Sarah’s appointment for the next day?
Phone the pharmacy/GP for advice?
Could the doctor do a phone consultation or home visit instead?
Rebook Sarah’s appointment for the next day? Cons: she feels she can’t wait that long
Phone the pharmacy/GP for advice? Cons: she may need more specialist advice, or they can’t give a prescription.
Could the doctor do a phone consultation or home visit instead? Pros: She doesn’t need to travel and the doctor can give her specialist advice and a prescription.
In the video below, carers talk about how they problem-solve together, with the patient, to overcome the challenges of breathlessness
Would you like to look at another support topic?
Page last reviewed: 08/05/2020
Prioritising
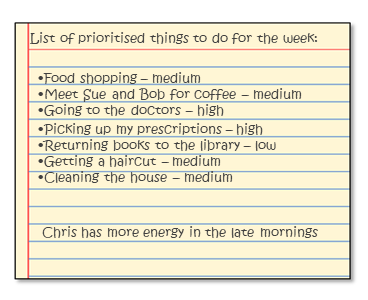
When you are caring for a patient who has limited energy, it is important to try and prioritise. Prioritising means deciding which jobs are most important and getting them done first. To help with this:
- Try writing down together, a list of everything you and the patient need to do in the next week. You’ll need to work around appointments and events that can’t be changed.
- Then decide together which are ‘high’, ‘medium’ and ‘low’ priority.
Have you tried...?
It can help to ask yourselves these questions
- Is this activity essential?
- Can it wait?
- Could someone else do it instead?
- Does it energize the patient? Does it revitalize them, or does it drain their energy away? E.g. seeing friends, watching a favourite film, or doing a hobby the patient enjoys
Ideas for how to decide which priority to give different activities:
Something like going to the doctors is high priority as it is essential to the patient’s health – it shouldn’t wait, it couldn’t be done by someone else and is energizing.
Returning books to the library would be low priority as it is not essential – it can wait, someone else could do it instead, and it doesn’t really energize the patient.
- Try to prioritise activities which are energizing and put those that are energy-draining lower down the list
- Try to think about times when the patient tends to have more energy and plan high priority activities for those times
- You may not get around to doing the low priority tasks, or it may be someone else does them for you instead. That is just fine because people do like to help. Give yourself permission to accept help from others.
- Once you have prioritised tasks, and agreed when the patient is most likely to be able to do them, you can start planning tasks for specific days
Would you like to look at another support topic?
Page last reviewed: 08/05/2020
Planning
Making plans can help but they can be hard to stick to when you are caring for someone. Breathlessness can be unpredictable.
- Planning ahead can help save precious energy
- Plan tasks for specific days, after you have prioritised the jobs you need to complete for the week.
- Try to space activities across the week to avoid doing things all in one day, or a few days close together
- You’ll need to work around appointments or events that can’t be changed. Try to book appointments for the time of day when the patient tends to have more energy, allowing time for getting ready and travel.
- Be flexible and try not to be too hard on yourselves if you need to change your plans. You may need to check and change your weekly plan several times during a week.
In the video below hear from carers and patients how they use planning to get important jobs done
Would you like to look at another support topic?
Page last reviewed: 08/05/2020
Understanding Breathlessness
This is the only section with two landing pages?
Add two boxes linking to either Understanding Breathlessness Cancer or Understanding Breathlessness COPD
Cancer + COPD specific content:
Also if this is of any help we were thinking of our site having functionality like this homepage – click on the ‘journey’ (e.g “ I have COPD” or “I have asthma”) that is relevant to you and only see content relevant to that journey: