If the person you are caring for dies, it can be a difficult time particularly if you were very close to them. You may have some strong feelings of grief and loss to cope with. There may also be a number of practical things you need to do at the same time.
Grief and bereavement
Grief and bereavement are words used to describe a range of emotions and physical symptoms that you can experience after someone dies
 Common changes you might notice in your body:
Common changes you might notice in your body:
- being tearful
- difficulty sleeping
- feeling less, or more, hungry and weight loss or gain
- lack of energy
- headaches
- tiredness
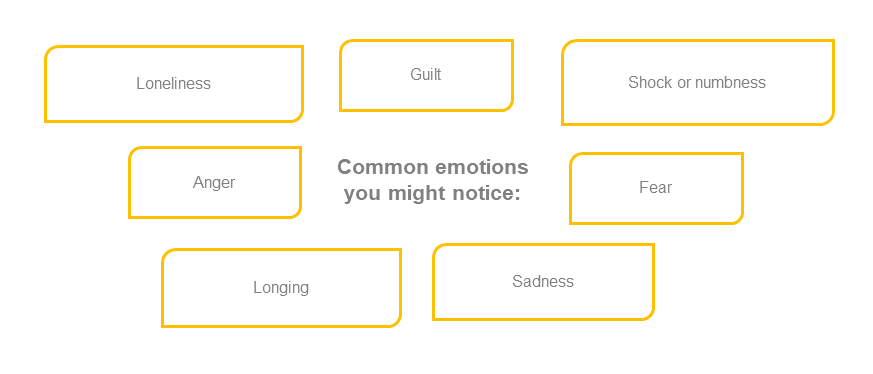
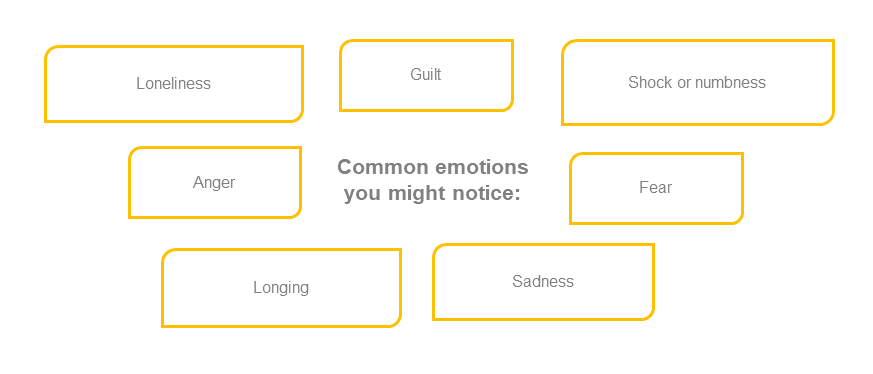
It’s normal to feel a wide range of emotions when grieving. You may have different feelings day to day, and even hour to hour. The way we feel grief is different from person to person. There is no wrong or right way to feel. While some carers can feel very strong emotions after a patient dies, others may feel numb, not quite taking in what has happened. They may even feel relief that the patient is no longer suffering. These feelings might last for days, weeks or months. It’s also common for feelings of grief to return around important anniversaries such as the patient’s birthday, the anniversary of their death or special holidays.

Speak with your doctor if you feel unable to cope with daily life and feel that these grief feelings are going on longer than you think they should.
It is not uncommon for carers to have these feelings even before the patient has died, as you miss the way things used to be before they were unwell, and you prepare for the loss to come.
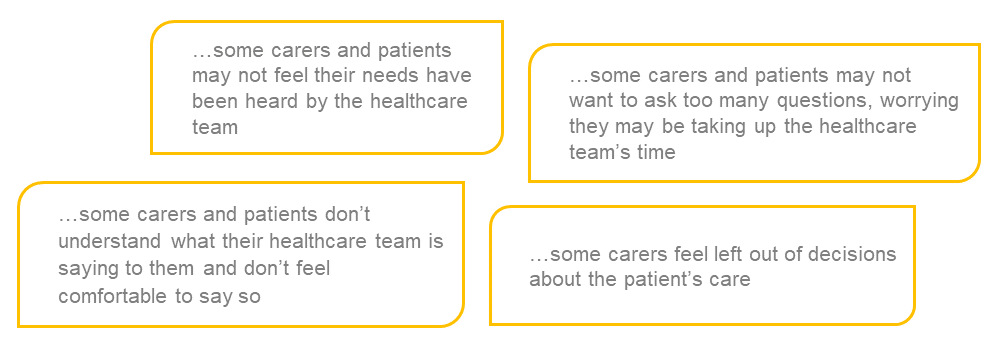
Some carers have mentioned feeling a ‘double loss’ as, once they are bereaved, they also lose relationships they have built up with professionals involved in the patient’s care.
Feelings of grief can also appear later as well. Grieving for the patient after they have died can be difficult when there are things to organise, leaving little time for carers to experience their feelings. Family and friends may also be visiting at this time which may keep you busy. This may mean that it is only when the practical things are done, and the family and friends have gone, that grief starts to show. Just be prepared for this.
It’s also important to be prepared for the possibility that some people may struggle to know what to say to you and may talk to you a bit less than normal.
‘It may not even hit them [carers] until a couple of days afterwards because you are up until that point, absolutely focused’
– ‘Brian’, former carer for his mother
What you can do to help yourself
Talking about the patient who has died, and what they meant to you, can help you work through grief. Talking to friends and relatives who knew the patient can be a good place to start. Talking with other people who have been bereaved – such as in a support group – or talking with a trained professional can also be very helpful.
‘You can get counselling – why not go and see. It could be something that will help you through it a little sooner or easier’
– ‘Diane’, former carer for her sister
Practical matters
There may be a lot of practical things to organise immediately after the death of the patient. It can help to know ahead what some of these might be, so you can feel a bit more prepared. Not all of these things will need to be arranged by you. If you find you are feeling overwhelmed by the amount of practical things that need to be organised, remember family and friends can help. Some practical things will need to be done by professionals.
Some of the main things that carers or family and friends may need to help organise include:
- letting the patient’s GP or community nurse know
- getting a medical certificate for cause of death – several copies if possible
- registering the death
- arranging the funeral
- managing wills and probate
- arranging the patient’s estate
- managing benefits – including carer benefits and how they may change
- reviewing your housing situation
- cancelling utilities, bank accounts and subscriptions
You can read more about what some of these practical things are and what is involved by visiting Carers UK – Practical Matters.
Some carers struggle to manage these practical things while they are grieving. Using the strategies of prioritising, planning, problem solving and looking after your own health might be useful. Remember that family and friends are likely to be around at this time, and will often want to help – make good use of them.
Planning a funeral ahead of time
Some carers and patients find that planning the funeral together, in advance, can be helpful. It may be reassuring for both the carer and patient to know that the patient’s wishes are being considered, and that things have been organised ahead of time. However, it is important to remember that not all patients and carers want to talk about the funeral together and some patients may prefer to plan their funeral on their own or leave it to others to arrange.
Moving on
After some time, most people notice their grief feelings becoming less intense and they can start to think about the future. They may also be able to start to think about some of the better times they shared with the patient, even while they were ill. While caring for someone with breathlessness can be challenging, some carers have told us that after a few months they have even been able to think about some of the positive things that have come from caring for the patient.
‘We got so close, closer than I thought we’d ever be. You think you’re close to someone, a sister or whatever and we felt we were pretty close but we both said we got so close, we talked about things we’d never talked about’
– ‘Diane’, former carer for her sister
Click here for a printable version of this page (PDF, 499KB)
Would you like to look at another support topic?
Page last reviewed: 16/06/2020

 Common changes you might notice in your body:
Common changes you might notice in your body:
 Please be advised: the following information in this topic is meant to help prepare you and the patient if things get worse. Some people can find reading and talking about this type of information upsetting.
Please be advised: the following information in this topic is meant to help prepare you and the patient if things get worse. Some people can find reading and talking about this type of information upsetting.